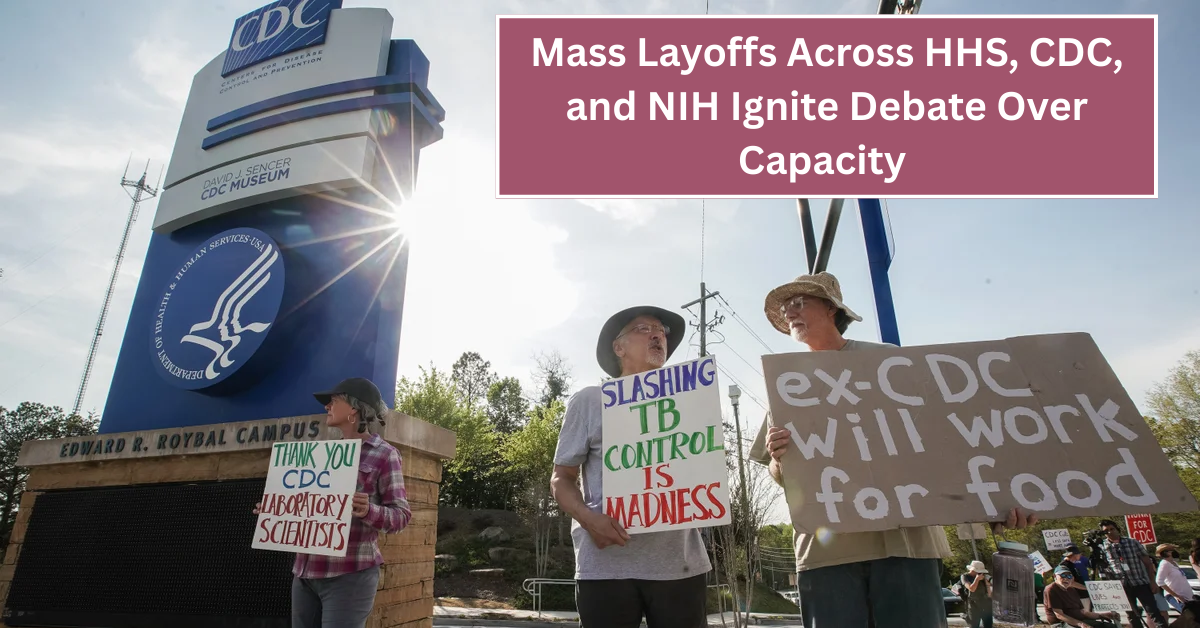
The recent wave of mass layoffs across key health agencies such as the Department of Health and Human Services (HHS), the Centers for Disease Control and Prevention (CDC), and the National Institutes of Health (NIH) has sparked significant concern among public health experts, government officials, and the general public alike. These cuts raise serious questions about the ability of these organizations to continue safeguarding the nation’s health in an era fraught with emerging health threats and ongoing challenges.
As these agencies undergo staffing reductions, debates have intensified around whether such decisions compromise critical health initiatives and emergency responses. The layoffs come at a time when the public’s trust in government-led health programs is paramount, and the demand for efficient, well-resourced institutions to manage health crises has never been higher.
Understanding the Scale of Layoffs in Federal Health Agencies
Mass layoffs have impacted thousands of employees across HHS, CDC, and NIH, weakening their operational strength. The scale of these reductions is unprecedented in recent memory and includes scientists, epidemiologists, and support staff, all vital to the daily functioning of public health systems.
With fewer personnel, these agencies face challenges in conducting research, monitoring disease outbreaks, and developing medical countermeasures. Staffing shortages may delay responses to public health emergencies and reduce the agencies’ capacity to address long-term health threats effectively.
Impact of Workforce Cuts on Disease Surveillance and Response
Disease surveillance is one of the fundamental roles of the CDC and HHS. Layoffs in these sectors reduce the workforce responsible for tracking infectious diseases, analyzing data trends, and issuing timely health advisories. This diminished capacity could delay the detection of emerging outbreaks or variants of diseases, placing the public at greater risk.
Moreover, with fewer epidemiologists and laboratory technicians, the speed and accuracy of diagnostic testing may suffer. Resource constraints can also limit the effectiveness of vaccination campaigns and public health education, essential in controlling the spread of communicable diseases.
Research Constraints at NIH Due to Reduced Staffing
The NIH is a global leader in biomedical research, contributing to advancements in treatments, vaccines, and health interventions. The workforce reductions have led to a slowdown in research projects, including those focusing on cancer, neurological disorders, and infectious diseases. This stall in innovation could have long-term implications for patient care and public health preparedness.
Less funding and fewer researchers also mean that high-risk, high-reward studies may be deprioritized, hindering breakthroughs that could transform medicine. The morale among remaining staff is often impacted negatively, which can further reduce productivity and creativity within the institution.
Public Health Programs and Community Outreach Facing Setbacks
Beyond research and surveillance, these agencies manage vital public health programs that directly affect communities nationwide. Workforce cuts risk scaling back initiatives aimed at preventing chronic diseases, promoting mental health, and improving maternal and child health outcomes.
Losing outreach staff undermines efforts to engage vulnerable populations, particularly in underserved or rural areas. This reduction in community-based work can exacerbate health disparities and leave some groups more exposed to the consequences of poor health education and prevention services.
Table: Overview of Layoffs and Potential Risks Across Agencies
| Agency | Estimated Workforce Reduction | Key Impact Areas | Potential Risks |
|---|---|---|---|
| HHS | Large-scale cuts including administrative and field staff | Health program management, policy implementation | Delays in program delivery, reduced oversight |
| CDC | Significant cuts among epidemiologists and lab personnel | Disease surveillance, outbreak response | Slower detection of outbreaks, weakened pandemic preparedness |
| NIH | Research staff reductions across multiple institutes | Biomedical research, innovation | Reduced research output, stalled medical advances |
Concerns Raised by Public Health Experts and Policymakers
Health experts and lawmakers have voiced concerns that these layoffs undermine the nation’s ability to prepare for and respond to current and future health emergencies. They argue that cutting frontline personnel during a period where global health threats continue to evolve is counterproductive and shortsighted.
Policymakers are debating whether the reductions are reflective of a broader trend of decreasing investment in public health infrastructure. Many call for increased funding and resources that would support a robust and agile health workforce capable of meeting 21st-century challenges.
The Role of Technology and Innovation Amid Staff Reductions
Some argue that advances in technology, such as artificial intelligence and automated data processing, could offset some of the impacts of reduced staffing. These tools can enhance disease modeling, streamline administrative tasks, and improve communication systems within agencies.
However, technology is not a complete replacement for human expertise, particularly in complex decision-making, field investigations, and community engagement. Therefore, while innovation is vital, it cannot fully compensate for significant workforce shortages.
Public Perception and Trust in Federal Health Agencies
Public trust in health agencies is closely tied to their perceived capacity to protect citizens’ health. Workforce reductions can erode confidence if people believe that these agencies lack the necessary resources to fulfill their missions. Maintaining transparency about the reasons for layoffs and future plans is crucial to preserve trust.
Effective communication with the public about ongoing health risks, preparedness measures, and resource allocation can help alleviate fears and foster collaboration between communities and health institutions.
Strategies to Strengthen Public Health Capacity Moving Forward
To address the challenges posed by mass layoffs, there is a growing call for comprehensive strategies that include increased funding, recruitment incentives, and enhanced training programs. Strengthening partnerships between federal agencies, state and local health departments, and private sectors can also improve resource sharing and operational efficiency.
Investing in public health infrastructure, modernizing data systems, and supporting workforce development are key priorities aimed at rebuilding the capacity to manage health emergencies and advance medical research.
Conclusion
The mass layoffs across HHS, CDC, and NIH represent a critical moment of reflection on the nation’s commitment to public health. As these agencies strive to maintain their essential functions with fewer resources, the debate over America’s ability to protect its citizens intensifies. Ensuring a strong, well-supported public health workforce remains vital for tackling current challenges and safeguarding health equity for future generations.
Building resilience in public health infrastructure requires careful balancing of budget constraints and the undeniable need for capable professionals. With strategic investments and thoughtful policy decisions, the United States can reinforce its defenses against health crises and foster innovation that benefits all citizens.